- LEARN MORE: The faint 'mark' on a woman's nose which was later discovered to be cancer
Emily Haley received her father's light skin color, and throughout her entire life she was careful to apply SPF to both her face and body.
She knew skin cancer had been possible due to her parents' background with skin cancer, yet when an unusual mark showed up on her forehead, she assumed it was a zit.
The ad was released just over a year back and ran for several months, although Haley thought nothing of it She thought it would disappear like any other pimple over time. It began to turn red in December 2024.
She mentioned it to her dermatologist during her following appointment, Dr. Hooman Khorasani, a specialist in skin conditions and aesthetic surgery located in New York. After examining the area through a microscope, Dr. Khorasani found it concerning. He observed specific blood vessels that aren’t typically present in regular pimples.
Following the collection of a tiny piece of tissue and conducting several tests, Dr. Khorasani informed Haley with devastating information: the lesion was basal cell carcinoma (BCC), the most frequent type of skin cancer. This condition arises due to particular genetic changes in skin cells, although these alterations may occur randomly, they typically stem from prolonged exposure to ultraviolet rays.
Learning that she has cancer from her physician was frightening, yet he reassured her that since the disease was detected at an early stage, her outlook was very positive.
Basal cell carcinoma progresses gradually and rarely spreads. If detected at an early stage, localised instances are usually treatable, boasting nearly a 100% five-year survival rate — one of the highest among all types of cancer.
Haley's operation was planned to take place several weeks following her diagnosis. Dr. Khorasani would carry out a Mohs micrographic surgery on her brow, which entails carefully stripping away minute sections of tissue, consistently examining the layers beneath a microscope until every malignant cell has been removed.

Even Haley's physician had difficulty accepting that the tiny red spot was malignant. Haley was just 31 years old, whereas the demographic typically affected by this form of cancer falls between the ages of 70 and 79.
However, Haley had a familial background with this condition on both sides. Her mother contracted the same type of cancer in her 60s, roughly seven years prior, while her father experienced pre-cancerous skin lesions during his 50s.
She told Women’s Health My family background along with my pale complexion made it seem nearly inevitable that I would encounter a comparable destiny.
But in trying to keep myself safe, I followed my sunscreen regimen consistently, avoided sunbeds entirely, and saw a dermatologist every year for checks against skin cancer.
'Experiencing basal cell carcinoma even with my healthy lifestyle (and being diagnosed much earlier in life compared to my parents) was unexpected. It served as a clear reminder that skin cancer can affect anyone at any moment.'
At first, she worried about the scar that would come from the Mohs procedure. A certain amount of scarring is normal, yet for someone working in the beauty sector as a marketer, reducing visible evidence of her illness was crucial.
"The condition of my scar and the multiple dressings wrapped around it inevitably attracted notice, yet not always the sort I wished for," she remarked.
I wasn't always eager to explain myself or admit that I was going through cancer. Still, I find solace in knowing that this period of my life will eventually come to an end.
BCC occurs much more frequently compared to its dangerous relative melanoma, with approximately 5.4 million cases diagnosed annually.
Closely associated with sunlight, this type of cancer occurs when cells in the outermost layer of the skin start dividing excessively, resulting in a reddish area that may feel sore or have an itching sensation.
Physicians usually can eliminate it through Mohs surgery, increasing the survival rate to 99 percent.
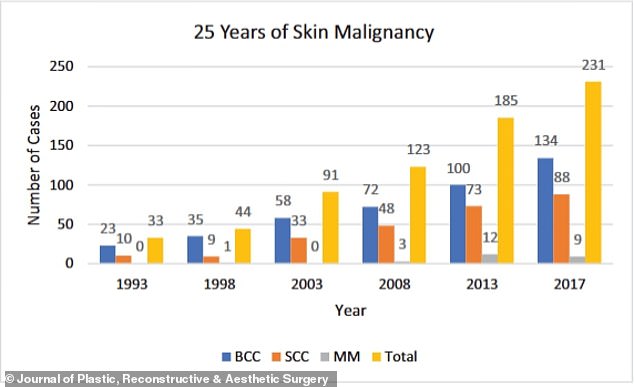
It is increasingly prevalent as well. As reported by the NIH, incidence rates have increased by 20 to 80 percent over the past three decades, particularly within the expanding elderly demographic.
Dr. Khorasani keeps conducting outpatient treatments to reduce the appearance of scars, such as Dermabrasion and CO₂ laser resurfacing, which eliminate the top layer of skin and encourage collagen production.
Vascular lasers help minimize redness by focusing on blood vessels, whereas Bellafill injections address elevated or sunken scars by filling them in. Botox may stop scarring from spreading by loosening surrounding muscles.
Haley stated, "Still, the recovery following the operation hasn't consistently gone smoothly (my scar tends to appear particularly reddish right after sessions), yet on better days, I can confidently say that you'd barely notice the scar because of the support provided by my physician and his staff."
Ever since the incident, she has been far more careful with skincare, frequently reapplying sunscreen during the day, putting on caps and protective clothing when at the shore, and scheduling regular check-ups with her dermatologist every half-year, following guidelines from the American Cancer Society.

The medical facility where she receives treatment employs artificial intelligence to examine detailed images of her entire body in order to check for any malignant growths. Thus far, she shows no signs of cancer.
'After many months of wearing different hats and scarf covers, I no longer care about others' opinions of me or my appearance,' she stated.
When individuals inquire about my scar, I'm pleased to recount my experience. As long as being open assists at least one person detect an issue sooner, safeguard their skin, or feel less isolated, it will have been entirely worthwhile. In the meanwhile, I'll continue wearing my preferred hat.
Read more
Post a Comment for "I Thought a Bump Was a Pimple—Then I Got a Shocking Diagnosis"