
Scientists report that the blood from a U.S. man who intentionally injected himself with snake venom for almost 20 years has resulted in an unprecedented antivenom.
The antibodies discovered in Tim Friede's blood have demonstrated protection against lethal amounts from various species in laboratory animals.
Existing treatments must correspond to the particular species of venomous snake that someone has been bitten by.
However, Dr. Friede's 18-year quest might represent a major advancement toward developing a universal antivenom for all snake bites—a condition responsible for up to 14,000 deaths annually and causing three times as many individuals to require amputations or suffer from lasting disabilities.
Overall, Mr. Friede has experienced over 200 bites and more than 700 administrations of venom he extracted from some of the globe’s most lethal serpents, such as various types of mambas, cobras, taipans, and kraits.
His original aim was to develop resistance against snake venom to safeguard himself during interactions with them, chronicling his adventures on YouTube.
However, the ex-truck mechanic mentioned that he had "botched things up badly" initially after suffering from two consecutive cobra bites that put him into a coma.
“I had no desire to die. I wasn’t keen on losing a digit either. Missing work was also not an option,” he shared with Positivibemind.com.
Mr. Friede’s drive stemmed from his desire to create improved treatments for those globally, stating: “It simply turned into my way of life, and I continuously strived with all my might—specifically for the individuals located 8,000 miles away from me who succumb to snakebites.”
I would really like to obtain some of your blood.
Currently, antivenom is produced by introducing minor amounts of snake venom into creatures like horses. The animal’s immune system combats the venom by generating antibodies, which are then extracted and utilized as therapeutic agents.
However, venom and antivenom must be precisely tailored since the toxins present in a venomous bite can differ significantly between various species.
Even within the same species, there can be significant variation; for example, antivenom produced using snakes from India. is less effective versus the same species in Sri Lanka.
A group of scientists started looking for an immunological defense known as broad-neutralizing antibodies. Rather than focusing on the aspects of a toxin that make it distinct, these antibodies zero in on the sections shared across various types of toxins.
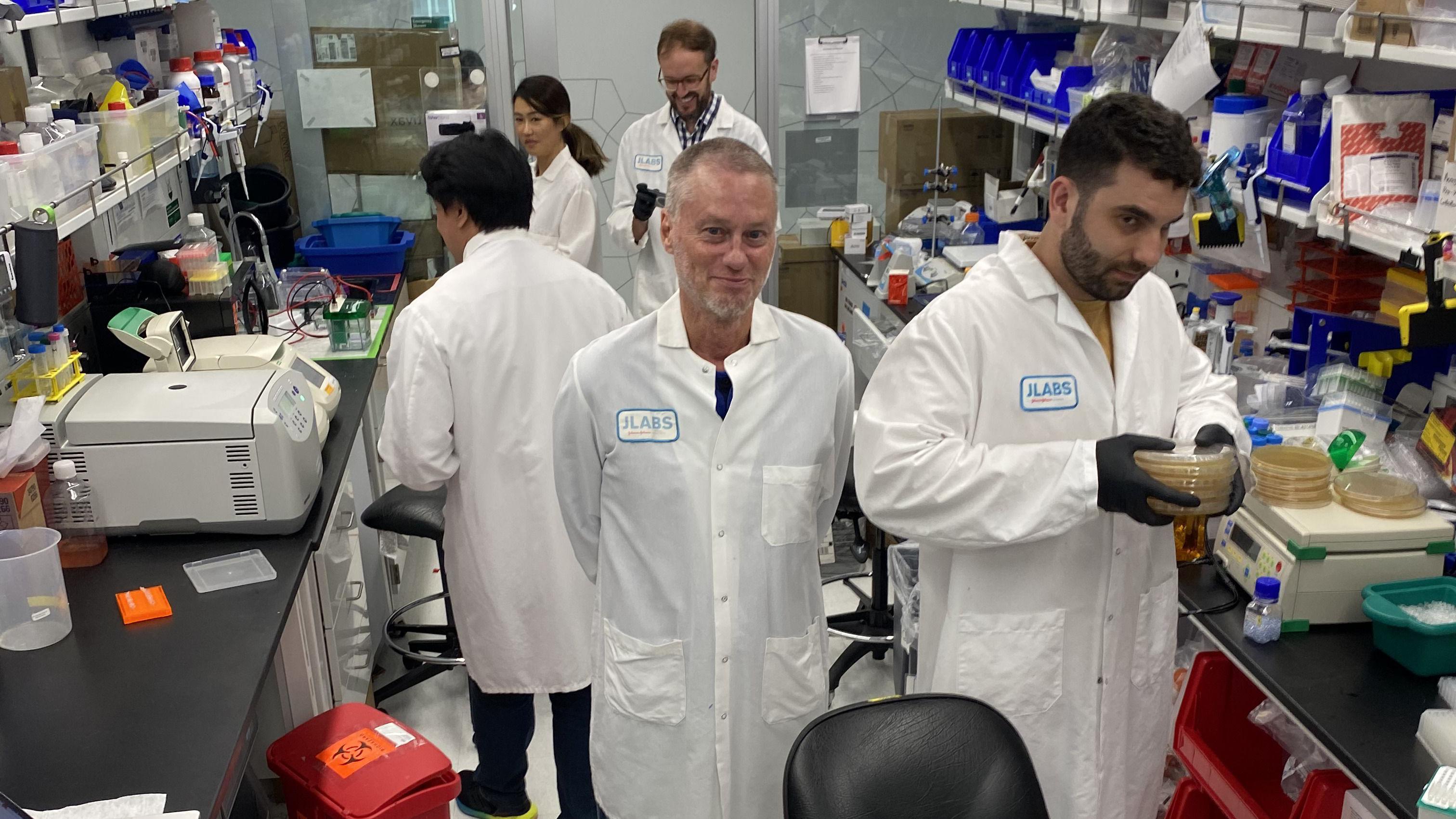
It was then that Dr. Jacob Glanville, who serves as CEO of the biotechnology firm Centivax, stumbled upon Tim Friede.
"As soon as I heard about it, I thought 'if anyone in the entire world has produced these broadly neutralizing antibodies, it would definitely be him,' so I got in touch," he explained.
The initial phone call went something like this: 'This could be an odd request, but I'm really interested in obtaining some of your blood.'
Mr. Friede concurred, and the project received ethical clearance since the research entailed drawing blood instead of administering additional venom.
The study centered on elapid snakes—one of the two groups of poisonous serpents—including species like coral snakes, mambas, cobras, taipans, and kraits.
Elapids primarily use neurotoxins in their venom, which paralyses their victim and is fatal when it stops the muscles needed to breathe.
Researchers picked 19 elapids identified by the World Health Organization as being among the deadliest snakes on the planet. They then began scouring Mr Friede's blood for protective defences.
Their work, detailed in the journal Cell , discovered two widely effective antibodies capable of targeting two categories of neurotoxins. To create their antivenom mixture, they included an additional drug aimed at countering a third category of toxins.
During tests with mice, the mixture allowed them to survive lethal amounts of venom from 13 out of 19 types of poisonous snakes. The rodents experienced some level of defense against the rest of the six varieties.
This unprecedented range of coverage offers protection against numerous species, as stated by Dr. Glanville, likely including many elapid snakes for which effective antivenoms do not currently exist.

The group is working on improving the antibodies even more and testing whether incorporating a fourth element might result in complete immunity to elapid snake venom.
The second category of snakes – the vipers – depend more heavily on hemotoxins, which target the bloodstream, as opposed to neurotoxins. Snake venoms generally consist of about a dozen major types of toxins, including cytotoxins that cause cell death.
"Within the next 10 to 15 years, I believe we will develop an effective solution for each category of these toxins," stated Professor Peter Kwong, who is part of the research team at Columbia University.
The search goes on within Mr. Friede's blood specimens.
"Tim's antibodies are truly remarkable – he trained his immune system to achieve this extensive recognition," stated Professor Kwong.
The ultimate aim is to develop either a universal antivenom capable of addressing all snakebite cases, or two separate injections—one for elapid bites and another for viper bites.
Professor Nick Casewell, who leads the Centre for Snakebite Research & Interventions at the Liverpool School of Tropical Medicine, stated that the extensive protection demonstrated is "definitely innovative" and offers "solid proof" that this method could be viable.
Undoubtedly, this piece advances the discipline into an exhilarating new trajectory.
However, he warned that significant work remained ahead and the antivenom required thorough testing prior to being administered to humans.
However, for Mr Friede, arriving at this point "gives me a sense of satisfaction."
I am contributing positively to humanity, which holds great significance for me. This makes me feel proud. It’s quite impressive.
Post a Comment for "Miracle Antivenom: Man's 200 Bites Lead to Breakthrough Treatment"